What is Laparoscopic Sleeve Gastrectomy ?
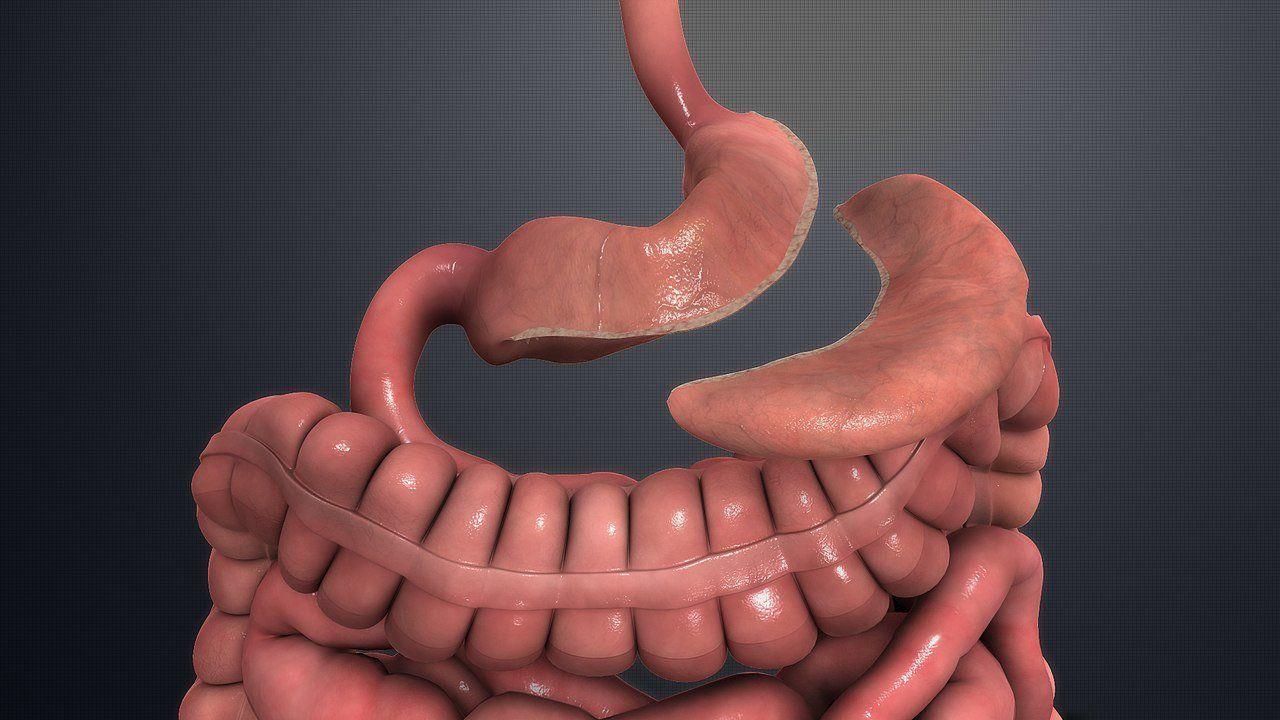
Sleeve gastrectomy is technically a procedure involving removal of the large part of the stomach that functions as a reservoir. With the procedure, the volume of the stomach that is normally1.5-2 liters is reduced to 30-150 ml (roughly the size of a banana). It does not involve placement of a foreign body into the abdomen, as in gastric banding surgery. The goal is to reduce the amount of food that can be consumed at a time; however, no intervention is made to the digestive system’s natural mechanism in such a way as to reduce absorption.
Even in the United States, where once gastric bypass surgery was considered to be the gold standard, the rate of sleeve gastrectomy revision was %24 in the late 2011s but today it is over %60. On the other hand, gastric bypass decreased from 62% to 37% and gastric band decreased from 7.5% to 0.8% during this period.
The main advantages of sleeve gastrectomy includes that it does not change the natural mechanism of the digestive system and therefore does not lead to vitamin and mineral deficiencies, does not cause dumping syndrome, causes less reflux complaints than gastric band surgery, and does not involve the replacement of any foreign matter into the body; while its most important disadvantages include the risk of bleeding and leakage through a relatively longer stapler, i.e. incision line and the fact that it is a non-reversible procedure, contrary to gastric band surgery.
Although the non-reversibility of sleeve gastrectomy seems initially to be a negative condition, the effects of sleeve gastrectomy on the daily life are definitely at acceptable levels after the surgical risks in the early postoperative period are overcome.
Complaints such as nausea, vomiting, and pain are extremely rare if the patient’s compliance with the eating rules is good, after the sleeve gastrectomy operation performed in accordance with the technique. Frankly, reflux is the only significant effect of sleeve gastrectomy I that may affect the comfort of life in the postoperative period. Almost one in every 5 patients experiences reflux in the first postoperative year but this rate drops to 3% after 3 years.
Moreover, the process of the patient’s adaptation to the sleeve stomach is better than the adaptation process in gastric band surgery. The side effects of sleeve gastrectomy are less than that of gastric bypass and larger operations. Some long-term studies comparing these surgical procedures, such as the Swedish Obese Subjects (SOS) trial, have shown that the average weight loss is equivalent to that of gastric bypass and much better than that of gastric band. In comparison with all other procedures, duodenal switch procedure enables patients to lose more weight. In terms of overall short-term risks, the risk of sleeve gastrectomy is equal to that of gastric bypass, higher than that of gastric band, and lower than that of duodenal switch. In terms of long-term risks, its risk is lower than that of all other procedures. The feeling of hunger is lower than that felt after gastric band and gastric bypass procedures.
In term of the improvement of type 2 diabetes, the effectiveness of the sleeve gastrectomy is similar or equal to that of gastric bypass. However, there are studies indicating that diabetes can recur in the long term. In terms of operation time, sleeve gastrectomy is more advantageous than bypass. In terms of quality of life, the both procedures have similar effects.
How Does Sleeve Gastrectomy Act?
During the procedure, approximately 85% of the stomach is removed in such a way as to remain only a thin tube-like stomach with a thickness equal to that of your thumb. Thus, the amount of food that can be consumed at a time is considerably reduced so that the patient feels satiety earlier. This is the restrictive effect of the procedure.
However, sleeve gastrectomy is not only a restrictive operation, but also a procedure with hormonal and metabolic effects. The removed part of the stomach is the part that produces the hunger-triggering hormone Ghrelin. Removal of this part reduces the amount of appetite-inducing hormone in the blood, and generally leads to suppressed appetite.
Since the natural mechanism of the digestive system is not intervened in, digestion and absorption functions continue normally after sleeve gastrectomy. Therefore, it poses a much lower risk of vitamin and mineral deficiencies in comparison with surgical procedures that intervene in absorption.
How Much Weight is Lost After Sleeve Gastrectomy?
Obesity is not just an imbalance between the caloric consumption and the caloric intake, as initially thought. There are many hormonal mechanisms underlying how people who reached the obesity stage can lose weight by just reducing the caloric intake.
Sleeve gastrectomy is a surgical procedure that can provide you with a very powerful weapon for your fight against obesity, by resetting such mechanisms. However, it cannot be effective alone, like all other obesity surgeries. When supported with a healthy dietary system and exercise, you can be enabled to lose 60-80% of your excess weight within the first postoperative period. Of course, there is the risk of not being able to lose adequate amount of weight and even regain weight when rules are broken and old bad habits are resumed.
How is Sleeve Gastrectomy Performed?
Sleeve gastrectomy is performed with the laparoscopic method, i.e. by making 4 or 5 small incisions on the abdomen. The operation takes 30 to 45 minutes on average. Of course, this is also related to previously performed surgeries or anatomy. The hospitalization period is usually 2 or 3 days.
Is an Intense Pain Felt after Sleeve Gastrectomy?
All surgical procedures involve pain to a certain extent. However, pain is at minimal levels in laparoscopic procedures. In fact, not much pain is felt in any place other than the trocar entries. At our center, our patients usually feel a slight pain (or no pain) because of the facts that incision sites are numbed with long-acting painkillers, and that devices called Patient-controlled analgesia (PCA) infusion pump, intended for providing extra doses of painkiller depending on the patient’s request, are routinely used. Many of our patients do not request even the routine painkillers from the second postoperative day.
How Is The Follow-Up Process After Sleeve Gastrectomy?
In sleeve gastrectomy, as in all other surgical procedures for obesity, the success increases directly with strict postoperative controls and observations. Therefore, your first visit will be done 7 to 10 days after surgery, on average. In that first visit, investigations will be made to find the clues of early complications of the surgical operation, and to ascertain whether the postoperative nourishment and other life functions are normal. Our nutritionist will see you before surgery, in the first postoperative days, on the 15th day when you will begin to consume mashed foods instead of liquid foods, and after the first postoperative month, when you will begin to consume solid foods.
Your routine controls will be done in the 1st-3rd-6th-12th-18th-24th
postoperative months. In these controls, primarily sugar and insulin levels, liver enzymes, vitamins and mineral levels as well as renal functions will be checked through blood tests. If any deficiencies are detected in these, special supportive treatments will be determined. Our nutritionist will also monitor your body composition and confirm whether you lost weight without muscle loss.
In addition, if you have undergone operations due to severe metabolic conditions such as uncontrolled diabetes, our endocrinologist will want to see you at the frequencies to be determined by him/her. If a psychotherapy program had been followed before the surgery, it will be asked to be followed again after surgery. Our patients living outside our city or abroad can have their routine tests performed and send us their results to enable us to follow-up them, as long as all goes well. You can establish one-to-one communication with our team with video conferences via Skype, phone and e-mail.
Am I Eligible for Sleeve Gastrectomy?
If according to the criteria of the International Federation for the Surgery of Obesity & Metabolic Disorders (IFSO) you have a weight problem within the surgical limit, if you currently have vitamin-mineral deficiencies that may cause problems with bypass and other procedures, if you have a disorder requiring the use of or an anti-inflammatory drug that may cause a problem during bypass surgery, if you have Crohn’s disease or a story of abdominal surgery, if you have heart or lung problems that may cause a problem with an operation that takes a long time, and if you are at the threshold of super morbid obesity, sleeve gastrectomy will definitely be suitable for you as the first option. The age range suitable for sleeve gastrectomy is 12 to 79 years of age.
In What Situations Might Sleeve Gastrectomy Be Unsuitable For Me?
If you have Type 2 diabetes, especially to an extent that requires insulin use, if you have a body mass index (BMI) of 50 or greater, and if you complain of a severe reflux, bypass may be a better option for you. Let us remind again the facts that sleeve gastrectomy can be performed as the first step, and it would be a better option to perform the main surgical operation after achieving weight loss to a certain extent. Since 20% of patients with reflux experience more reflux complaint after sleeve gastrectomy, such patients should be careful when making decision on this procedure. The condition associated with the chronic reflux called Barrett’s esophagus is a definite contraindication for sleeve gastrectomy. In other words, sleeve gastrectomy should definitely not be performed on patients with Barrett’s esophagus.
How is the Cost of Sleeve Gastrectomy?
The cost of Sleeve Gastrectomy in the United States ranges from 13,000 to 30,000 USD. Many insurance companies have included these surgical procedures in their insurance coverage. Unfortunately, private insurance companies in our country are still insisting on keeping bariatric surgery out of their insurance coverage. On the other hand, the social security institution makes a payment that does not cover even the cost of the device used in such operations.
