In this article, we will cover the basic features of mini gastric bypass, indications, patient selection, technical details, complications and controversial issues, its use as revision surgery, and all issues that need to be known about postoperative follow-up.
Mini Gastric Bypass (Single Anastomosis Gastric Bypass) Basic Information:
History of Mini Gastric Bypass Surgery:
Mini gastric bypass surgery was first applied in 1997 by Dr Robert Rutledge who is a trauma surgeon at North Carolina University Hospital, for a patient who was injured in the abdomen with a firearm. This continuity of gastric anatomy, which is performed because of necessity, has led to the development of the idea of mini gastric bypass. Reconstruction of the stomach is similar to the old Billroth II surgery, but a longer and narrower stomach pouch is created.
In 2000, Dr. Ruthledge presented mini gastric bypass data at the annual congress of American Obesity and Metabolic Surgery. Many surgeons faced serious resistance as they confused this surgery with the old-style Mason loop bypass surgery that caused bile reflux and dangerous leaks.
In 2005, Dr. Eric Demaria from the University of Iowa published his article “Complications of mini gastric bypass and revision to Roux-en-Y”, which examined 32 patients from 5 different hospitals in North Carolina. However, most of the cases in this article were performed by Dr Steven Olchowski, who was not trained by Dr Ruthledge, and contrary to the technique, the stomach pouch was too short. Following the controversy, Dr Ruthledge holded his surgical career in the United States and undertook the mission of teaching the correct mini gastric bypass technique all over the world, collaborating with certain surgeons in all countries.
Dr. Murat Ustun has the first contact with Dr. Ruthledg. He has been provided the Platinum Instructor certificate by Dr. Ruhtledg. Dr. Murat Ustun organizes mini gastric bypass certification courses with Dr Rutledge for the correct recognition and performance of mini gastric bypass surgeries in Turkey.
The first of these was held in Adana Regional Hospital in 2018, where, in addition to theoretical training, primary and revision mini gastric bypass surgeries were performed by Dr Ruthledge and Murat Üstün in the live broadcast, and bronze certificates were given to more than 100 participants.
In the Long-term results, which have been examined by more and more publications over time, have shown the superiority of mini gastric bypass over sleeve gastrectomy and Roux-en-Y surgeries in terms of safety, quality of life, permanence and ease of revision.
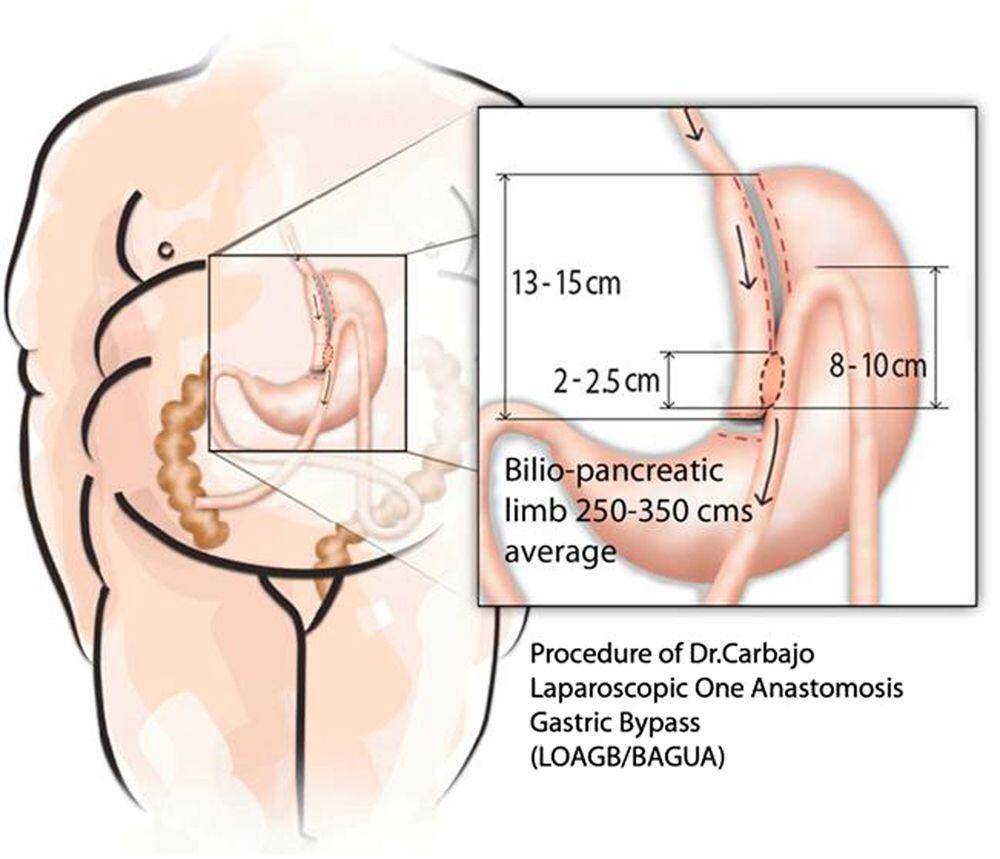
In 2002, Prof. Miguel Carbajo from Spain started to implement a modified version of the mini gastric bypass after reviewing the publications of Dr Ruthledge. This modification involves fixing an 8-10 cm afferent bowel loop to the gastric pouch to take advantage of gravity to reduce reflux.
Both bariatric surgery options were presented by Rutledge Carbajo’s invitation to the Spanish Obesity Association meeting in 2004. Carbajo named its modification as OAGB (One Anastomosis Gastric Bypass) or Bagua (Bypass Gastrico de una Anastomosis).
In August 2012, the first mini gastric bypass consensus meeting was held in Paris under the leadership of Dr Ruthledge, Kular and Deitel. The second meeting was also held in Paris in November 2013. In 2014, IFSO (International Society for Obesity Surgery) organized the first mini gastric bypass course during its annual conference in Montreal. The Mini Gastric Bypass Club was established at the Vienna Congress in 2015 under the leadership of Kular, Deitel and Rutledge. The club, whose first member from our country is also Dr. Murat Üstün, meets every year.
In 2018, IFSO reported that it accepted mini gastric bypass as one of the main surgical techniques, but demanded that the name “mini” not be used, and that it be called a Single Anastomosis Gastric Bypass. Discussions on this subject still continue.
Mini Gastric Bypass or Single Anastomotic Gastric Bypass?
Dr Mario Musella summarizes the differences of Dr Rutledge’s mini gastric bypass technique from the old Dr Mason loop bypass technique as follows:
-Mason loop bypass creates a wide and short, horizontal stomach pouch. Therefore, reflux of bile from the intestine that brings bile to the stomach and esophagus is the most important problem.
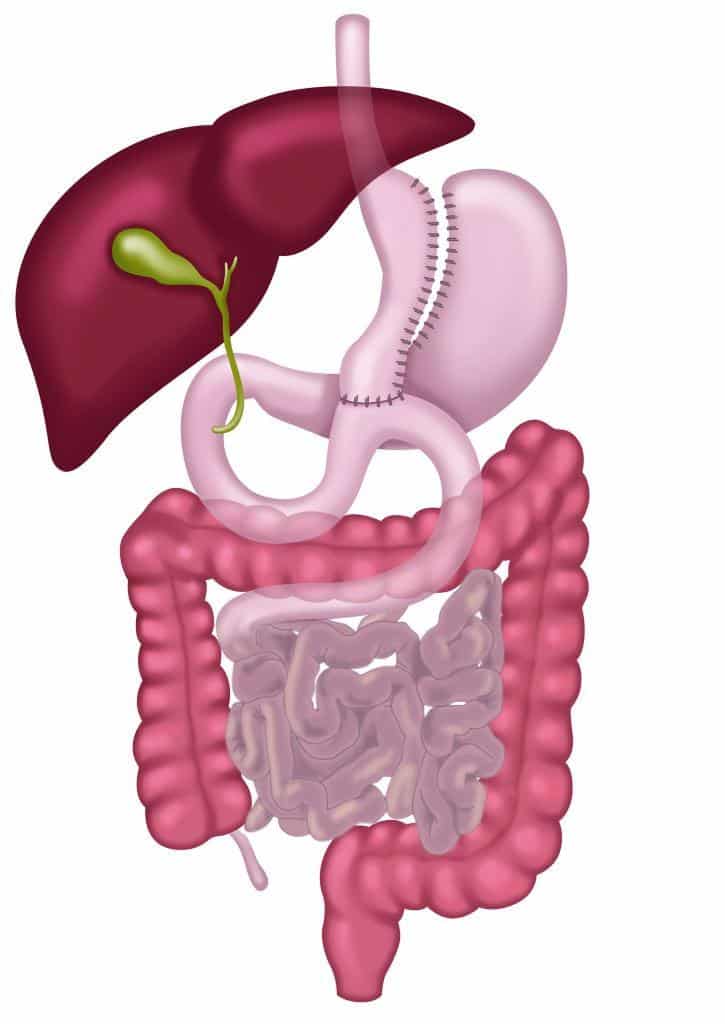
In the mini gastric bypass technique, the separation of the stomach, called Crow’s foot, starts at a distance of 3-4 cm from the stomach exit, ie pylorus. A long stomach pouch separated from the body and antrum junction of the stomach is joined with a small intestine 200 cm from the Treitz ligament. Unlike the Roux-en-Y gastric bypass method, no difficulty is encountered in the upward movement of the intestine and the anastomosis is made in front of the colon, that is, the large intestine.
Dr Musella points out the importance of the stomach pouch being long and narrow. The stapler should be placed no more than 1 cm behind the calibration tube and unlike sleeve gastrectomy, there is no need to approach the stomach-esophagus junction more than 1-2 cm. Thus, in gastric tube surgery, this area where leaks are most common is avoided and the risk of leakage is almost eliminated.
There are also differences between mini gastric bypass and anti-reflux Bagua technique. Bagua technique creates a latero-lateral anastomosis between the stomach pouch and the intestine. Preparation of the stomach pouch also begins horizontally. Jejunum is fixed to the stapler line in the stomach pouch with 6-10 stitches. The entire bowel distance is measured and the gastrojejunostomy is performed at the intermediate level. Biliopancreatic and common ducts are almost equal in length (250-350 cm) and 10-50 cm for each BMI value is counted as a bypassed small intestine. Care is taken to ensure that the common channel is at least 250-300 cm.
Mini gastric bypass and Bagua are not the same surgery, especially due to the difference in bowel measurements. However, it is in the same surgery group and we can call this group pre-pyloric single anastomotic gastric bypass.
The Numbers of Mini Gastric Bypass Applied Around The World
IFSO president Prof Almino Ramos reports a dramatic increase in the number of mini gastric bypass surgeries around the world in recent years. Although sleeve gastrectomy is still the most preferred method, while all other methods are gradually decreasing, only the number of primary and revision mini gastric bypass is increasing. However, the increase in the number of surgeries is not equal. While Britain, Israel, Egypt, Switzerland, Australia and Argentina adapted much faster, there is still a prejudice against the MGB in America.
Referring to the information in the IFSO Obesity Surgery Database (2019), Prof Ramos reports that there is evidence that mini gastric bypass is superior to Roux-en-Y and gastric sleeve surgery in weight loss in super-morbid obese patients. Despite these advantages, more research is needed to increase postoperative musculoskeletal pain.
As a result, mini gastric bypass is now one of the mainstream obesity surgery methods. Not only the number of cases, but also the number of research and publications is gradually increasing. This increase reached 31% in 2018. The technical guidelines of mini gastric bypass are also very clear. According to the survey we conducted with 58 members of the MGB Club, these key points are:
– Calibration tube diameter should be between 34-40 mm and should not change according to age or BMI.
– The use of stapler line boosters are not standard.
– Gastrointestinal anastomosis should be 45 mm.
– Splitting the large omentum is not routine and should be done if necessary.
– Closing the Peterson space is not routine.
– Measurement of total bowel length is not routine.
– The minimum BMI range for non-obese diabetic patients is 25-30.
– Hiatal hernias above 5 cm should be closed routinely in the same surgery.
– Roux-en-Y revision should be considered in severe reflux cases.
– Routine postoperative gastric protector use is around 3-6 months.
– Use for lifelong vitamins are multivitamin, calcium, iron, vitamin D and B12 injection every three months.
– Increasing the bypass distance is the most suitable revision option for heavy weight-gain.

The Biggest Advantages of Mini Gastric Bypass:
Ideal obesity surgery is a method that can be performed with minimal risks and complications, providing permanent weight loss, correcting comorbid diseases, improving the quality of life and extending life expectancy. In this context, mini gastric bypass stands out as a method that is technically easy to apply and revision when there is a problem. It is possible that it will be the most common revision surgery in the coming years. MGB is an effective and powerful surgery, provided that it is applied with the right technique and its basic principles are not violated.
Even Prof Mal Phobi, who was a supporter of Roux-en-Y gastric bypass and even had his own band produced and performed banded bypass surgery, came to the congress in 2010 to discuss BPD-DS and banded bypass as the best bariatric surgery. He said that after the presentations of Ruthledge and Kular, his ideas about mini gastric bypass had changed.
Phobia, which started as a consultant at Mohak Bariatric and Robotic Surgery Center in India in 2016, shared the results of 2765 mini gastric bypass cases. Accordingly, revision to gastric bypass was required in only three cases due to bile reflux and in five cases due to excessive weight loss and hypoproteinemia. There were no deaths due to protein malnutrition in 4500 cases. Anemia and marginal ulcer rates are not higher than normal bypass. Bile reflux and newly developing reflux rates are below the gastric sleeve.
After performing 7000 gastric bypass and 3000 from other obesity surgeries, Mal Fobi says that mini gastric bypass is technically easy to apply and is a very effective method in super morbid obese patients. “Contrary to all personal and political prejudices, mini gastric bypass is a superior surgery than banded gastric bypass, although it is difficult for me to say.” he adds.
There are relative contraindications for mini gastric bypass. Such as cirrhosis, severe reflux, extensive gastric hernia, severe inflammatory bowel disease, stage I-II obesity, heavy smokers, patients with postoperative follow-up problems.
Who Is Suitable For Mini Gastric Bypass Surgery?
How Should the Patient Selection Be?
Mini-gastric bypass is an operation that has a restrictive effect but can be placed between Roux-en-y and biliopancreatic diversion, which is a more complex surgery. The rules in other bariatric surgery methods are also valid in patient selection for MGB, but there are also patient subgroups where mini-gastric bypass is particularly suitable.
-Age and BMI: Since excellent results have been reported in young adolescents (13 years) and elderly patients, all patients who are suitable for bariatric surgery and whose health conditions are suitable are candidates for MGB. However, attention should be paid about absorption-reducing distance in elderly patients and should be kept a little shorter. Moreover, mini-gastric bypass also has excellent results in super-morbidly obese patients, and if the absorption-reducing portion is kept as high as 60%, it can provide results comparable to a much more complex surgery, biliopancreatic diversion.
– Metabolic comorbidities: Patients with severe abdominal (central, visceral) obesity and / or advanced metabolic syndrome are particularly suitable candidates for MGB due to their excellent metabolic effects. Its high metabolic efficiency makes mini gastric bypass an excellent option for Type 2 diabetes patients, regardless of their body mass index. It has been proven that mini-gastric bypass provides long-term improvement or improvement in patients with advanced disease, and this effect is above the sleeve gastrectomy and RnY bypass.
– Reflux and Hiatal Hernia: With or without esophagitis (including non-dysplastic Barrett’s esophagus), obese patients with reflux disease are suitable candidates for mini gastric bypass due to its pressure-reducing effect.
-Small Intestine Condition: Small intestines must be free in MGB surgery, as it includes small intestine anastomosis. Small intestines should be freed carefully in patients with adhesions due to previous intra-abdominal surgeries. In cases of “frozen pelvis” where only the small intestine cannot be freed, both mini-gastric bypass and all mixed procedures involving the bowel are contraindicated. Although some experts consider cases where the small intestine is shorter than 3.5 m is a contraindication for MGB, it is not a problem if the entire small intestine can be measured and properly bypassed.
-Revision Surgery After Other Unsuccessful Surgeries: After unsuccessful restrictive surgeries such as gastric band and gastric sleeve, mini gastric bypass has been shown to be an excellent option in revision. Considering the popularity of sleeve gastrectomy nowadays, it can be predicted that revision surgery from the gastric tube to mini gastric bypass will be the most frequent revision surgery in the next ten years. Also, since it is an anti-reflux procedure, mini-gastric bypass may be a second option in cases of reflux after sleeve gastrectomy. Its effectiveness on reflux is similar to Roux-en-Y, but it is more effective in long-term and permanent weight loss.
-Special requirements: Obese chronic alcohol consumers and smokers should quit these at least 6 months before surgery. An eradication period of at least 3 years will be fine if there is any drug addiction.
Patient selection is key in optimizing mini gastric bypass results, but it is not that different from other surgeries. Although surgical risks are higher in super and super-super obese groups, mini gastric bypass is a very good alternative in these patients.
What Should Be The Expected Weight Loss After Mini Gastric Bypass?

The fact that it successfully combines the restrictive effect with the absorption-reducing effect and the nutritional comfort is higher, makes mini gastric bypass one of the most powerful methods compared to other obesity surgeries. The greatest weight loss after mini-gastric bypass occurs in the first year and 70% or more of the excess weight is lost. Literature information shows that although weight loss slows down, it continues to plateau in the second and third years and the excess weight loss rate remains at the level of 75-70% in 8-10 years.
Many publications show the superiority of mini gastric bypass compared to sleeve gastrectomy. Carbajo and his team, Demonstrated that it is superior to Roux-en-Y gastric bypass and sleeve gastrectomy in the long term. There is no significant difference between sleeve gastrectomy and RnY bypass in 1-2-5 years of follow-up. Shivakumar and his team, Reported that mini-gastric bypass was ahead in terms of improvement in comorbid diseases, quality of life and BAROS score, although there was no significant difference between gastric tube and mini-gastric bypass in terms of weight loss at 36-month follow-up.
Comparative studies between mini-gastric bypass and Roux-en-Y gastric bypass demonstrated the superiority of mini-gastric bypass at 5 and 10 years of follow-up, with only one randomized study reporting equal. It has proven to be more effective than sleeve Roux-en-Y gastric bypass in super obese patients.
Dr Fawal and Dr Chetan Parmar also reported superior results than RnY in terms of weight loss. Fawal also added that he achieved more successful weight loss after restrictive methods in revision surgery. In WJ Lee’s comparative study, when revision was made after sleeve gastrectomy, mini gastric bypass resulted in weight loss that doubled Roux-en-Y. Some other studies report that weight loss is near in the first year, increasing in favor of the MGB group after the second year.
Mini gastric bypass is definitely more effective than Roux-en-Y gastric bypass and sleeve gastrectomy in terms of weight loss and improvement of comorbidities. Because it is a more metabolic surgery, therefore, care should be taken against the higher risk of malnutrition. Although it is now a recognized surgery by IFSO, the balance between bile reflux and protein malnutrition must be precisely adjusted when determining bowel lengths.
Results Related to Age and Body Mass Index:
There are many obesity surgery options available, and these are applied at varying rates according to literature support, patient characteristics, surgeon experience, and surgical trends in each country. In the Israeli sample, data collected from 31 centers were evaluated. Mini gastric bypass has been implemented in Israel in 2014. The numbers have increased steadily, it has now become the most popular surgery in the country, accounting for 46% of all obesity surgeries. All other methods tend to decrease.
The reasons for the decrease in gastric sleeve surgery in Israel are stapler line leaks, weight gain and Barrett’s esophagus due to reflux. Mini gastric bypass is preferred to Roux-en-Y as an easier, less complex, faster and more effective method. In addition, it is relatively easy to apply in super-super obese, and its effectiveness is unquestionably superior to both methods. Although there are few publications on patients with a body mass index below 35, it is in terms of weight loss and resolution of metabolic complications.
Successful results similar to Roux-en-Y are obtained.
In geriatric patients, that is, in the elderly patient group, MGB stands out in terms of operative morbidity and mortality and permanent weight loss despite relative sedentary life after surgery. In adolescents, mini gastric bypass provides effective weight loss and improvement in comorbid diseases, and causes less medium and long-term complications compared to sleeve gastrectomy, gastric band and RnY bypass.
How is the Improvement in Comorbid Diseases with Mini Gastric Bypass?
The initial doubts about mini-gastric bypass are completely a thing of the past and it is now a valid method of bariatric surgery. Many studies have proven its success on comorbidities and in some cases it has been shown to be superior to other methods.
In Wang’s study comparing mini gastric bypass with sleeve gastrectomy, better results were obtained with mini gastric bypass in terms of weight loss and improvement in Type 2 diabetes, hypertension and sleep apnea. In another study, Wang compared mini gastric bypass with Roux-en-Y bypass and proved the superiority of mini gastric bypass in terms of both weight loss and improvement in Type 2 diabetes.
DeLuca examined two different studies comparing mini-gastric bypass with gastric sleeve. The first was the study of Seetharamiah et al. No difference was reported in terms of weight loss, improvement in hypertension and quality of life. However, MGB provided better results in the improvement of Type 2 diabetes after 1 year. Another study is the Ruiz-Tovar study, and it has been shown that MGB is superior to the gastric sleeve in terms of improvement of Type 2 diabetes, hypertension and dyslipidemia in the short and long term.
In 2005, Lee et al. Compared the Roux-en-Y with mini gastric bypass in terms of improvement of co-morbid diseases. After two years, MGB had improved at least RnY level. Five years after surgery, MGB patients continued to remain within the normal body mass index, while RnY patients progressed to the obesity group.
Therefore, mini gastric bypass provides better results than either sleeve gastrectomy or Roux-en-Y bypass in obesity-related diseases. More randomized controlled studies are needed to increase the evidence in the literature.
Reflux and Gastric Hernia:
There is a parallel relationship between obesity and reflux. In mini-gastric bypass, the gastrointestinal junction comes into contact with a mixture of enzymes such as food and gastric juices, bile, and pancreatic secretions. Although these fluids reach gastritis in the stomach and esophagus, it is one of the most criticisms of mini gastric bypass that they may cause reflux esophagitis. The most serious fear is that reflux can be triggered by mini gastric bypass and lead to esophageal cancer. However, gastric pouch or esophageal cancer has not been reported in mini gastric bypass operations except for 1 case.
Of course, in the presence of a hernia, it is logical to repair the hernia so that the stomach pouch does not slide up. In cases with severe reflux, it may be appropriate to evaluate the adequacy of the lower esophageal sphincter with advanced examinations such as pHmetry, impedance studies, and manometry. However, there are very few reports in the literature regarding reflux after mini-gastric bypass.
Mini gastric bypass is a low-pressure system, so concerns about reflux are not as intense as before. Bile gastritis may be more common, but it is not clear whether this is a pathological event.

Mini Gastric Bypass and Quality of Life:
The quality of life is significantly lower in obese individuals. This includes the physical, mental and social status, and with obesity surgery, these values improve significantly more than other treatment methods. Moreover, quality of life is directly related to the amount of weight lost, and improvement in mental status is multifaceted, from reduction of depression symptoms to increased self-esteem.
In the study of Lee et al., Social function, physical condition and emotional state were questioned, and significant improvement was reported in all patients. In the study of Bruzzi et al. Evaluating the postoperative GIQLI score, social, psychosocial and physical functions improved significantly in the surgery group.
Taha and Abuzeid reported significant improvement in their physical condition, relationships, depressive symptoms, antidepressant use, self-confidence and sexual activities in their study, in which they evaluated 1520 patients.
Compared to other surgical methods, mini gastric bypass provides a simpler technique, a safer postoperative period, and a significant improvement in quality of life.
How is the Preparation for Mini Gastric Bypass Surgery?
As with all other bariatric surgery methods, correct patient selection, preparation and training are key to achieving the best result. All patients should first be evaluated for suitability for surgery and examined by cardiology and chest diseases. Preoperative laboratory tests, especially including some vitamin and mineral levels, should be performed. Deficiencies that need to be corrected should be corrected before surgery. Finally, all patients must stop consuming carbonated drinks, alcohol and cigarettes before surgery.
The most important factor in achieving excellent results in the long term is patient education. Patients’ having detailed information about their surgery and being aware of what they should do after surgery increases the success. They have to know what to eat, how and when to eat and what to avoid. This information is given by our bariatric dietician in the preoperative preparation period. However, every patient who consents to the operation by signing the informed consent form should also know that it is their responsibility to be informed about this issue. Having the same information with the family, starting with realistic expectations and following postoperative recommendations make it easier to complete the process without any problems.
It is very important for your long-term success that you come for regular check-ups, follow our helpful posts on social media and our Obesity Support group.
Who Cannot Have Mini Gastric Bypass Surgery?
In fact, there are certain contraindications that apply to other obesity surgeries:
-Unacceptable risk of anesthesia
-Pregnancy
Known cancer
Active intra-abdominal infection
Liver cirrhosis Child C
Unstable psychopathological conditions
Active drug addiction
By the way, there are some relative contraindications for bariatric surgery:
Inadequate treatment of a preexisting endocrine problem
Smoking
-Low socio-economic status (at a level where postoperative nutritional needs cannot be met)
Anemia and nutritional deficiencies
Special conditions that may prevent mini gastric bypass surgeries in particular:
Crohn’s disease and inflammatory bowel diseases. Since it is not known exactly how these autoimmune diseases affect the small intestine, gastric sleeve surgery should be preferred in these patients and intervention to the intestine should be avoided.
Primary short intestine, that is, the total intestine length is shorter than 350 cm or shortened by surgery for some reason.
When applied correctly, mini gastric bypass is a safe and effective procedure, but standardization of the technique is imperative. When the technique is strictly followed, the possible complications are almost non-existent.
Standardization of Mini Gastric Bypass Technique:
The current IFSO chairman, Dr Lilian Kow, states that laparoscopic bariatric surgeries can take an average of an hour or longer in difficult cases. It is common to experience positional problems in cases with severe obesity. For this reason, mini gastric bypass stands out with its technical ease and speed, especially in super morbid obese cases.
Forming the Gastric Pouch (New Stomach):
In mini gastric bypass surgery, the new stomach pouch should have an average length of 18-20 cm. While the stomach pouch is being formed, the level called incisura should be passed behind the stomach, and the process should be continued through the 36 F calibration tube. The procedure should be completed before entering too much into the stomach-esophagus junction. The narrow and long stomach pouch is the most important technical detail that will prevent bile reflux. However, there is no study on how much stomach length will be sufficient to prevent bile reflux. However, in less than 40% of the cases, reflux of bile to the stomach pouch is observed, whereas reflux to the esophagus is observed in only 3% of cases. This rate is the same as those with reflux esophagitis that is more advanced than stage A.
Gastrointestinal Anastomosis:
Dr da Silva from Brazil states that despite the excellent results of mini gastric bypass, there are serious criticisms of bile reflux into the stomach and especially bile reflux into the esophagus. Mini gastric bypass has a very different technique than Billroth II known to classical surgeons. Intestinal distance of 30-40 cm created in Billroth II is more than 150 cm in mini gastric bypass. There are also differences between mini gastric bypass and Carbajo version, such as intestinal length that reduces absorption, and anti-reflux sutures. While the entire intestine length should be measured in Carbajo Single Anastomosis Gastric Bypass, this is not required in mini gastric bypass.
The bowel loop must be anticolic and antegastric, that is, it must be located in front of the stomach and large intestine. It should be formed isoperistaltic, that is, parallel to bowel movements. However, while Carbajo wanted the anastomosis to be created in the anterior stomach wall, no difference was found between the two models in clinical studies. However, Da Sİlva also believes that the posterior anastomosis is more functional and enables the gastric pouch to empty more easily. This also makes cleaning possibly biliary material easier. Gastrointestinal anastomosis should be side-to-side, posterior, approximately 30-35 mm.
Stapler-Cartridge Recommendations and Stapler Line Reinforcement:
Although more bleeding was reported with Ethicon Echelon in studies comparing staples, it is not clinically significant. The issue of stapler line strengthening is still controversial and there is no consensus. Although there are methods such as using fibrin glue, suture, butress material to strengthen the stapler line, they are methods whose benefits and harms have not been fully proven. Therefore, it is important to decide according to the characteristics of the case. In summary, the statements of the centers saying that they perform safer surgery by adding any method are incompatible with science.
Determination of Absorption-Reducing Intestinal Distance:
Kamal Mahawar from the UK states that in the past decades surgeons thought that Roux-en-Y bypass was effective with its restrictive and absorption-reducing properties, but as the absorption-reducing effect maximized the benefits of the procedure, the absorption-reducing distance was gradually extended and the concept of distal gastric bypass was born.
It is known that only 11% of the total calorie reduction after Roux-en-Y bypass is due to the absorption-reducing effect. In addition, it has been determined that the Roux-en-Y surgery shows the most beneficial result in a biliopancreatic length of 100-200 cm. Our experience with Roux-en-Y shows that bypassing the intestine more than 150 cm does not provide significant improvement in clinical results. Longer biliopancreatic length leads to increased nutritional complications. Therefore, Mahawar argues that the intestinal distance should not be more than 150 cm in a single anastomotic gastric bypass.
Closing the Mesenteric Gap in Mini Gastric Bypass:
One of the biggest advantages of mini gastric bypass surgery over Roux-en-Y is the avoidance of a second intestinal-intestinal anastomosis and the risk of internal hernia is almost 0. This opening, defined by Dr. Petersen in the 1900s, occurs because we separate the intestine in the Roux-en-Y bypass, but such a procedure is not required in the MGB. Therefore, closing the Petersen defect, which is one of the most difficult parts of the surgery, is not mandatory in mini gastric bypass.
Considering that more than 30,000 mini-gastric bypasses are performed in the world, the rate of internal hernia is found to be 1 in 5,000 on average. In Roux-en-Y, this rate increases up to 5 percent in the long term. There are only 4 reports published on MGB and internal hernia. However, internal hernia should be suspected in the presence of unexplained abdominal pain.
Mini Gastric Bypass Complications, Diagnosis, Prevention and Treatment:
Comparison of Roux-N-Y Gastric Bypass and Mini Gastric Bypass:
Mini gastric bypass has become the most widely used obesity surgery in the world after sleeve gastrectomy and Roux-en-Y gastric bypass. Numerous studies show that mini gastric bypass is an advantageous operation in terms of improvement in early postoperative complications, weight loss and comorbid diseases as a more metabolic operation.
There are 3 randomized controlled trials in the literature comparing Mini Gastric Bypass with Roux-N-Y Gastric Bypass. According to Lee’s study published in 2005, it is reported that mini gastric bypass causes fewer complications, there is no significant difference in weight loss in two years, and anemia is seen slightly more, according to the results of 2-year follow-up.
According to the wider Ruiz-Tovar study published in 2019, it is stated that there is no significant difference in terms of surgical risks, but mini gastric bypass provides better weight loss and better control in diabetes, dyslipidemia and hypertension. The YOMEGA study of Robert et al., Also published this year, shows that mini gastric bypass surgery times are shorter and early complication rates are similar. Two-year weight loss was not different between the two groups. While there is a similarity between type 2 diabetes recovery rates, complete recovery of diabetes is much higher in mini gastric bypass patients. (60% vs 38%) Nutritional complications were seen at a higher rate in mini gastric bypass patients.
Current literature shows that mini-gastric bypass can be performed in a shorter time, it has a higher effect on weight loss and metabolic comorbidities than Roux-en-Y gastric bypass, and in return, more nutritional complications and anemia may be encountered. The risk associated with bile reflux has not yet gone beyond the level of discussion, and further studies are needed.
Solving Problems Related to Mini Gastric Bypass by Surgery
Today, perioperative imaging methods and diagnostic examinations enable surgeons to be informed and prepared about the problem before entering the operating room. Thus, morbidity, mortality and complication rates are reduced.
The risk of encountering long-term problems that need to be corrected surgically after mini-gastric bypass is very low. In case of intraabdominal bleeding, classical surgical methods and diagnostic laparoscopy are gold standards. The bleeding stapler line will solve the problem by placing stitches, applying clips and using hemostatic agents. Sutures and omental flaps can also be used in acute marginal ulcer bleeding. Likewise, gastric pouch leaks and anastomotic leaks can be treated with sutures and omental flap, unlike gastric sleeve.
Leakage and Bleeding in Mini Gastric Bypass Surgery
As with all methods of obesity surgery, postoperative acute bleeding is one of the most common postoperative complications. If the bleeding is due to the stapler line, it may be into the digestive system or into the abdominal cavity. The dissected omentum can also be a source of kaama. If the bleeding is not very severe, it can be managed conservatively, ie with blood transfusion and follow-up. Sometimes it can be resolved by endoscopic methods.
The total major complication rate is around 2.7%, and bleeding constitutes 0.9% of it. (Carbajo) Again, according to Chetan et al., In a series of 12,807 patients, the bleeding rate requiring blood transfusion, endoscopic procedure or repeat laparoscopy is 1.12%.
In his series of 900 cases, Pacheco specified the most frequent bleeding focus as the stapler line, but only 2 cases required blood transfusion, and no patient required re-intervention.
Authors report different figures on the leakage rate. Carbajo reports 1%, Rudledge 1.1% and Chevallier 0.6%. Chetan examined 12,807 cases and found the leakage rate to be 0.96%.
More interestingly, Tovar reported the risk of leakage from 0 in mini-gastric bypass to 2% in sleeve gastrectomy and 1.5% in Roux en Y gastric bypass. He reported the bleeding rate closely. In our series, only 1 leak and 1 acute bleeding requiring laparoscopy developed in 450 cases. Suture treatment was sufficient in the leak, and in bleeding, the anastomosis line was reconstructed since the stapler line was focal.
Gastric Ulcer
Gastric ulcer development in mini gastric bypass is not much different from RnY. (Jammu) This rate varies from 0.5% to 5%. The main factors are smoking and the use of NSAID group painkillers. In addition, excessive acid production, alcohol, steroid use, anticoagulant use and H. pylori infection may also cause marginal ulcers.
Upper digestive system endoscopy, ie gastroscopy, is the most important method for diagnosis and biopsy should be taken from different parts of the stomach to evaluate H.pylori infection. Also, the presence of gastro-gastric fistula should be investigated at endoscopy, and signs of erythema or perforation around the anastomosis should be evaluated. Complicated, non-healing, obstructing, bleeding, penetrating or perforated marginal ulcers, that is, puncture, require surgical intervention.
In this case, if a perforation is detected, suturing the hole and applying a jejunal or omental patch on it is a good solution. Absorbable sutures and negative drains should be used. Sometimes the gastrojejunostomy needs to be completely rebuilt. Braun anastomosis or Roux-en-Y reconstruction can be used to deflect bile.
The best way to prevent these complications is avoiding anastomotic ischemia during the first surgery, creating a long gastric tube, and paying attention to tension-free gastrojejunostomy. Full recovery is achieved with early diagnosis and timely intervention.
Mini Gastric Bypass and Bile Reflux Discussion
The enterohepatic circulation of bile acids, their role in digestion and absorption, their metabolic effects and their close relationship with the microbiota are well known. After all types of gastric bypass, the circulation of bile acids changes. A slight decrease in bile absorption in the biliopancreatic intestine is one of the basic principles of mini gastric bypass surgery. The role of saffron in stomach cancer is clearly exaggerated.
In gastric bypass where a longer biliopancreatic leg is created, proximal bile acid absorption may occur before the digestive process begins. Since bile acids are pre-absorbed, a lower proportion of bile is present in the common channel into which food is added. For this reason, these surgeries are bile preserving surgeries and the bile acid pool will not decrease in the long term. Diarrhea, called collagenic diarrhea, is one of the bad side effects of bile acid. However, it is not common after standard-compliant mini gastric bypass. Bile is not normally a carcinogenic substance. However, it can be a co-factor in cancer development. However, there is now indirect evidence that bile acids may be carcinogenic in humans.
The majority of gastric cancer cases reported after gastric bypass surgery have been reported in an idle remnant stomach. In mini gastric bypass cases, anastomotic cancer has been reported in 1 case worldwide.
Dr Peter Small from the UK reports that some clinicians have reported their reservations about stomach or esophageal cancer associated with chronic alkaline reflux, whereas it is quite clear that bariatric surgery only reduces the risk of cancer by triggering weight loss and metabolic changes. Accordingly, connecting the small intestine to the stomach in a loop fashion can lead to biliary gastritis. However, this has not been shown to cause dysplastic changes. Gastritis is often seen after Roux-en-Y surgeries, which are said to be less likely to reach the stomach pouch. However, in recent histological studies comparing Roux-en-Y and mini gastric bypass patients, the frequency of biliary reflux, biliary reflux index and Sydney system score were found to be similar. In summary, Roux-en-Y was not found to be superior to mini gastric bypass in terms of bile reflux.
H.Pylori is a more important factor and may be a precursor to some changes occurring. It may be H. Pylori infection, which is responsible for the increase in gastric cancer rate after Billroth II gastrectomy surgery. Before bariatric surgery, eradication therapy may be a reasonable method of prevention regardless of the type of surgery in HP-positive patients.
Reflux of alkaline bile into the esophagus and development of esophagitis following mini gastric bypass has not been shown to be a major problem. Moreover, the data even suggest that bile reflux into the esophagus may decrease after MGB surgery.
In summary, there is no clear data reporting risk in terms of cancer development after mini gastric bypass surgery, and these data cover the 20-year period following the surgery.
Almost half of the population today is at risk of cancer, and this risk increases with obesity. Surgeries that provide weight loss have been shown to reduce the risk of cancer. Therefore, we have to choose between our long-term concerns regarding postoperative and proven benefits. When it comes to mini-gastric bypass, there are no consistent data to suggest that bile reflux leads to an increased risk of cancer, as feared. Some of the reported cases of esophageal cancer are mostly related to purely restrictive surgeries such as gastric band and gastric sleeve. Regardless, bariatric surgeons must be very careful and regular in monitoring and reporting patients after all bariatric procedures.
Gastroesophageal Reflux Disease and Barrett Esophagus
Reflux frequency in the non-obese population is in the range of 15-20%. In obese individuals, this rate is estimated to be between 50-100%. Moreover, prolonged gastroesophageal reflux disease is associated with esophageal inflammation and metaplastic transformations in the healing phase. To protect itself, the esophageal mucosa transforms into the cylindrical epithelium covering the stomach, which is called intestinal metaplasia or Barrett’s esophagus. It is seen in 10% of severe reflux cases. The risk of developing esophageal cancer in low-grade dysplasia cases is calculated as 0.5-13% per year. In high-grade dysplasia, it reaches 5-20%.
Therefore, the presence of reflux disease or Barrett’s esophagus must be evaluated with preoperative endoscopy. In this way, the risk of complicated reflux disease can be prevented. If there are no signs of esophagitis on endoscopy, impedance Ph studies can be used to evaluate symptoms.
Biliopancreatic bowel length is the most important factor in malnutrition. In numerous studies of Mahawar et al., It was reported that this distance should be kept 150 cm and below. However, as this distance becomes shorter, the concentration of bile acids increases and the risk of biliary reflux will increase in parallel.
Lifestyle modifications and drug therapy are the first steps to effectively treat Barrett’s esophagus and reflux disease. Weight loss with obesity surgery is the main factor of improvement in reflux symptoms. H2 receptor antagonists, proton pump inhibitors (PPI) and sucralfate can be used to treat acid reflux. Many drugs have been tried to treat bile reflux, but some benefit has been achieved. These are ursodeoxycholic acid, bile acid sequesters, PPI, prokinetic drugs and Baclofen.
Roux-en-Y revision is recommended in the literature in case of reflux that cannot be stopped after mini-gastric bypass. In high risk cases, the surgery can be completely reversed.
Reduced Absorption and Protein Calorie Malnutrition
Schikora suggests that the positive effects of MGB are likely due to the longer intestinal distance. As the skipped bowel distance increases, the risk of malnutrition increases. Moreover, most of the patients experience nutritional deficiencies before surgery. For this reason, it is important to check these before surgery and to complete the deficiencies. The most frequently deficient values are B1, B6, B12, folate, iron, Vitamin A, Vitamin D, Vitamin E, Vitamin K, zinc and albumin. Macro and micronutrients are absorbed from different parts of the digestive system. Therefore, various nutritional deficiencies can be seen after bariatric surgery. For this purpose, patients should be closely monitored and any nutritional deficiency should be intervened before it gets deeper.
Mini Gastric Bypass and Patient Follow-up as Revision Surgery
Complications of the Biliary Tract After Mini Gastric Bypass
Although stone formation in the gallbladder is quite common (30-50%) following bariatric surgery, the rate of symptomatic gallstones requiring removal of the gallbladder is as low as 3.5-6.1% after gastric sleeve surgery and 6.1-10.6% after Roux-en-Y bypass. The rate of gallbladder surgery after mini-gastric bypass has been reported as 2%.
Because of the increased risk of stone formation in the gallbladder and the difficulty in reaching the bile ducts endoscopically after surgery, some authors recommend protective cholecystectomy in bypass surgery. The other group, which I am a part of, thinks that it is not necessary to have the bladder removed in the same session because of the preoperative ultrasound, removal of the bladder first if the stone is detected, and the relatively low risk of symptoms. 60-80% of patients with stones in the gallbladder do not show symptoms.
The use of Ursodeoxykolic acid is the routine application of the Istanbul Bariatric Center to prevent the formation of gallstones, especially during the rapid weight loss period. Available data suggest that it is not necessary to remove the gallbladder in the same session. In symptomatic stones, biliary surgery can be performed before bariatric surgery. The surgeon should perform the risk assessment and evaluate it in the same session or before.
Weight Recovery After Mini Gastric Bypass and Revisional Surgery Indications
After MGB, reoperation may be required due to leaks, strictures or ulcer perforation. It has been shown that successful results can be obtained with less invasive methods. In the literature, the rate of weight regain after mini-gastric bypass is low. In this case, the method called Triple Attack can be used for revision. This approach includes reducing the gastric pouch, narrowing the anastomosis diameter, and increasing the absorption-reducing bowel distance (one-third of the total bowel length). This approach is the routine method that we, as Istanbul Bariatric Center, apply in our Roux-en-Y revisions. (Click to watch the video)
Mini Gastric Bypass Revision Techniques
In mini gastric bypass, revision operations may be required for various reasons such as bleeding, stenosis, perforation, excessive weight loss, unstoppable malnutrition, weight gain, insufficient weight loss or reflux. To standardize the concept of weight gain:
– Recovery of more than 25% of the lost weight
-Returning 10 pounds or more after the lowest weight down
-5 BMI value recovery
For complications, revision to Roux-en-Y bypass may be an option. However, readjustment of bowel length according to total bowel distance will often solve the problem. Revision to completely normal anatomy is also possible in mini gastric bypass, and it can be easily performed by experienced hands.
Mini Gastric Bypass as Revision Surgery
There is an increasing demand for revision surgery for insufficient weight loss or weight regain, especially after restrictive surgeries. Although there are limited data in the literature, we see that the surgery is very safe when compared to the mini gastric bypass performed after restrictive surgery and primary MGB, but the quality of life is lower after revision. Again, in other studies, mini gastric bypass revision after gastric band surgery and sleeve gastrectomy seems to be extremely safe and effective. MGB offers more successful slimming than revision Roux-en-Y. However, anemia is a problem that should be followed in the long term.
SADI revision after sleeve gastrectomy is another type of revision that provides reliable and satisfactory weight loss. Mini gastric bypass offers results that are absolutely superior to Roux-en-Y and close to SADI in terms of revision surgery.
Patient Follow-up After Mini Gastric Bypass
Since there may be vitamin and mineral deficiencies in obese patients before surgery, these should be examined and completed before surgery. Things to be completed and done before the surgery:
-Vitamin B1, B12, D
-Calcium
-H.Pylori eradication
Endoscopy
Things to do after the surgery are:
– full biochemistry examination at the first year and 3th, 6th, 9th and 12th months.
– examination once in every 6 months a year (at the 2. Year)
-examination every year in once
-Vitamin B1, B12, D monitoring and supplementation if necessary
-Hb level, calcium, PTH monitoring and supplementation
-Liver function tests, monitoring of protein and albumin levels
– Early ultrasound for cholecystitis at 6th and 9th months.
– Endoscopy is recommended in 1st and 3rd years.
Stomach Protector Use After Bypass Surgery
Gastric-intestinal junction ulcers, called marginal ulcers, are a known complication after gastric bypass surgery. It has been reported in 1-16% of patients. Various researchers have reported similar rates after mini-gastric bypass. Stomach acid plays a role in the development of the disease. For this reason, most obesity surgeons routinely use stomach protectors after surgery.
The problem here is the intestinal mucosa, which is relatively vulnerable to acid attack. Some factors that cause ulcers are:
-Large stomach pouch (technical error)
-use of painkiller and smoking
-Mucosal malnutrition
– Gastrogastric fistula (passage of the acid produced by the remaining stomach to the intestinal junction)
-Foreign body reaction (stapler and stitches)
– Previous H. Pylori colonization
Although most bariatric surgeons routinely use gastric protector after gastric bypass surgery, there is insufficient evidence in the literature to support its benefits. Marginal ulcer formation can occur in the early and late stages. In early marginal ulcers, blood supply problems in the anastomosis may cause an increase in stomach acid in the late period. It is thought that the use of gastric protection after mini-gastric bypass may reduce marginal ulcer, but the duration of use is unclear. Many surgeons recommend it for 6 months. (Hamburg Consensus meeting-June 20
Ideal Multidisciplinary Follow-up
An effective, high quality, safe and comprehensive follow-up and care process is required after bariatric surgery. This can only be provided by experienced and well-equipped centers specialized in this field. Multidisciplinary follow-up both increases the success rates, improves the quality of life and provides faster recovery and recovery.
The multidisciplinary team includes internal medicine and endocrinology specialists, anesthetists, nephrologists, hepatologists, respiratory diseases specialists, gynecologists, cardiologists, endoscopists, psychologists and nutritionists specializing in obesity. This team ensures that the right patient is directed to the right bariatric surgery, that long-term weight loss is achieved and maintained, acute and chronic complications are immediately recognized and metabolic problems are corrected. For this reason, we recommend that you determine the center and surgeon you will be operated on not only on the basis of cost, but also by researching all these.
References:
Mahawar KK, Jennings N, Brown J, et al. BMini^ gastric bypass: systematic review of a controversial procedure. Obes Surg. 2013;23(11):1890–8. https://doi.org/10.1007/s11695-013-1026-8.
Musella M, Susa A, Greco F, et al. The laparoscopic mini-gastric bypass: the Italian experience: outcomes from 974 consecutive cases in a multicenter review. Surg Endosc. 2014;28(1):156–63. https://doi.org/10.1007/s00464-013-3141-y.
Kular KS, Manchanda N, Rutledge R. A 6-year experience with 1, 054 mini-gastric bypasses—first study from Indian subcontinent. Obes Surg. 2014;24(9):1430–5. https://doi.org/10.1007/s11695- 014-1220-3.
Chevallier JM, Arman GA, Guenzi M, et al. One thousand single anastomosis (omega loop) gastric bypasses to treat morbid obesity in a 7-year period: outcomes show few complications and good efficacy. Obes Surg. 2015;25(6):951–8. https://doi.org/10.1007/ s11695-014-1552-z.
Mahawar KK, Kular KS, Parmar C, et al. Perioperative practices concerning one anastomosis (mini) gastric bypass: a survey of 210
O’Kane M, Pinkney J, Aasheim E et al. BOMSS Guidelines on perioperative and postoperative biochemical monitoring and micro- nutrient replacement for patients undergoing bariatric surgery. Adopted by BOMSS Council September 2014. http://www. bomss.org.uk/wp-content/uploads/2014/09/BOMSS-guidelines- Final-version1Oct14.pdf Last Accessed on 7th July’ 2017
Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guide- lines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient—2013 update: cosponsored by American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic & Bariatric Surgery. Obesity (Silver Spring). 2013;21(Suppl 1):S1–27. https://doi.org/ 10.1002/oby.20461.
Lee WJ, Ser KH, Lee YC, et al. Laparoscopic Roux-en-Y vs. mini- gastric bypass for the treatment of morbid obesity: a 10-year expe- rience. Obes Surg. 2012;22(12):1827–34. https://doi.org/10.1007/ s11695-012-0726-9.
Mahawar KK, Carr WR, Balupuri S, et al. Controversy surrounding ‘mini’ gastric bypass. Obes Surg. 2014;24(2):324–33. https://doi. org/10.1007/s11695-013-1090-0.
Mahawar KK, Aggarwal S, Carr WR, et al. Consensus statements and bariatric surgery. Obes Surg. 2015;25(6):1063–5. https://doi. org/10.1007/s11695-015-1606-x.
Rubino F, Nathan DM, Eckel RH, et al. Metabolic surgery in the treatment algorithm for type 2 diabetes: a joint statement by inter- national diabetes organizations. Obes Surg. 2017;27(1):2–21. https://doi.org/10.1007/s11695-016-2457-9.
Gagner M, Hutchinson C, Rosenthal R. Fifth International Consensus Conference: current status of sleeve gastrectomy. Surg Obes Relat Dis. 2016;12(4):750–6. https://doi.org/10.1016/j.soard. 2016.01.022.
Mahawar KK, Borg CM, Kular KS, et al. Understanding objections to one anastomosis (mini) gastric bypass: a survey of 417 surgeons not performing this procedure. Obes Surg. 2017; https://doi.org/10. 1007/s11695-017-2663-0.
Mahawar KK. Key features of an ideal one anastomosis/mini- gastric bypass pouch. Obes Surg. 2017;27(6):1630–1. https://doi. org/10.1007/s11695-017-2673-y.
Carbajo MA, Luque-de-León E, Jiménez JM, et al. Laparoscopic one-anastomosis gastric bypass: technique, results, and long-term follow-up in 1200 patients. Obes Surg. 2017;27(5):1153–67. https://doi.org/10.1007/s11695-016-2428-1.
Kular KS, Prasad A, Ramana B, et al. Petersen’s hernia after mini (one anastomosis) gastric bypass. J Visc Surg. 2016;153(4):321.https://doi.org/10.1016/j.jviscsurg.2016.05.010.
Mahawar KK. Petersen’s hernia may be commoner after OAGB/ MGB than previously reported. Obes Surg. 2017; https://doi.org/ 10.1007/s11695-017-3001-2.
Mahawar KK, Sharples AJ. Contribution of malabsorption to weight loss after Roux-en-Y gastric bypass: a systematic review. Obes Surg. 2017;27(8):2194–206. https://doi.org/10.1007/s11695- 017-2762-y.
