Overview
Apollo Endoscopic Sleeve Gastroplasty (ESG) is an exciting development in obesity treatment that offers people a safe and effective alternative to the established weight loss options. Its main attraction is that it is non-surgical so people benefit from a lower risk profile and faster recovery time.
Endoscopic sleeve gastroplasty is a newer type of weight-loss procedure. Endoscopic sleeve gastroplasty reduces the size of your stomach using an endoscopic suturing device without the need for surgery. This procedure may be an option if you’re significantly overweight — a body mass index of 30 or more — and diet and exercise haven’t worked for you.
Endoscopic sleeve gastroplasty leads to significant weight loss. It helps you lose weight by limiting how much you can eat. And the procedure is minimally invasive, reducing the risk of operative complications.
Like other weight-loss procedures, endoscopic sleeve gastroplasty requires commitment to a healthier lifestyle. You need to make permanent healthy changes to your diet and get regular exercise to help ensure the long-term success of endoscopic sleeve gastroplasty.
Why it’s done
Endoscopic sleeve gastroplasty is performed to help you lose weight and potentially lower your risk of serious weight-related health problems, including:
- Gastroesophageal reflux disease
- Heart disease and stroke
- High blood pressure
- Sleep apnea
- Type 2 diabetes
Endoscopic sleeve gastroplasty and other weight-loss procedures or surgeries are typically done only after you’ve tried to lose weight by improving your diet and exercise habits. Endoscopic sleeve gastroplasty is less invasive and risky than other forms of bariatric surgery.
Who it’s for
Endoscopic sleeve gastroplasty is often an option for people who aren’t candidates for other bariatric surgeries. The procedure is available to people whose body mass index (BMI) is above 30 who haven’t been successful maintaining weight loss with other methods.
But endoscopic sleeve gastroplasty isn’t for everyone who is overweight. A screening process helps doctors see if the procedure might be beneficial for you. And you must be willing to commit to healthy lifestyle changes, regular medical follow-up and participate in behavioral therapy.
Endoscopic sleeve gastroplasty isn’t appropriate for anyone who has gastrointestinal bleeding, a hiatal hernia larger than 3 centimeters or who’s had prior stomach surgery.
Given that endoscopic sleeve gastroplasty is a new procedure, it might not be covered by your health insurance.
The operation itself
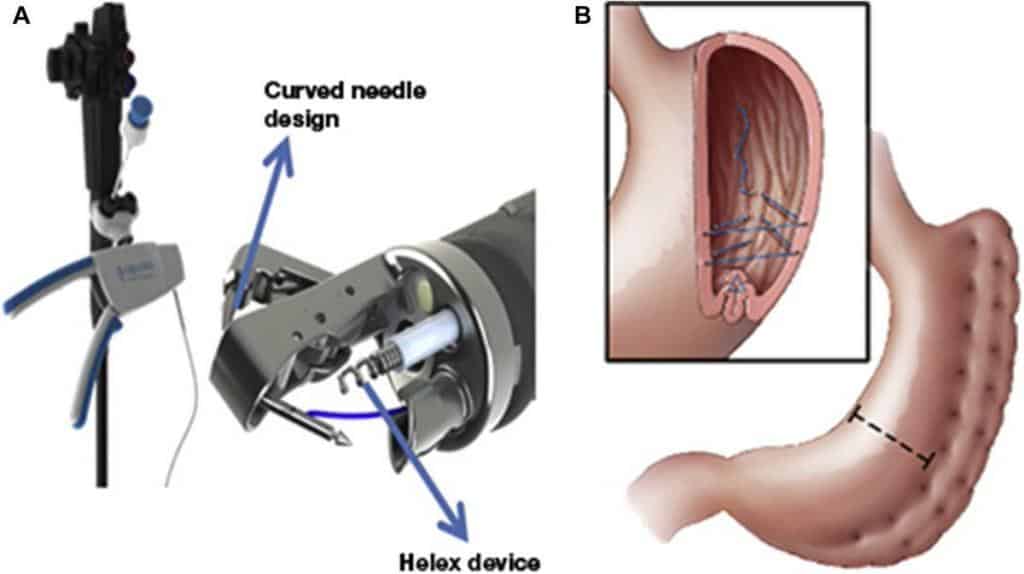
The ESG procedure is done using a device called an Overstitch; a device that is placed into the stomach through the mouth that enables us to place a number of sutures (stitches) inside the stomach to significantly reduce its capacity by up to 80%.
As the procedure requires about an hour to complete we do it under general anaesthetic for your comfort. However, unlike surgery, we do not need to make any incisions to access the abdominal cavity thus reducing the risk to you and enabling a faster recovery.
Risks
In early studies on endoscopic sleeve gastroplasty, the procedure has shown a favorable safety profile. Pain and nausea may occur for several days after the procedure. These symptoms are usually managed with pain and nausea medications. Most people feel better after two days.
In addition, although it’s not designed to be a temporary procedure, endoscopic sleeve gastroplasty can be reversed. In some cases, it can also be converted to bariatric surgery.
Because the procedure is still new and not in wide use, questions remain about its long-term effectiveness and risks.
How you prepare
If you qualify for endoscopic sleeve gastroplasty, your health care team will give you specific instructions on how to prepare for your procedure. You may need to have various lab tests and exams before surgery. You may have restrictions on eating, drinking and which medications you can take. You also may be required to start a physical activity program.
It’s helpful to plan ahead for your recovery after the procedure. For instance, arrange for help at home if you think you’ll need it. Recovery from endoscopic sleeve gastroplasty generally only takes a day or two.
What you can expect
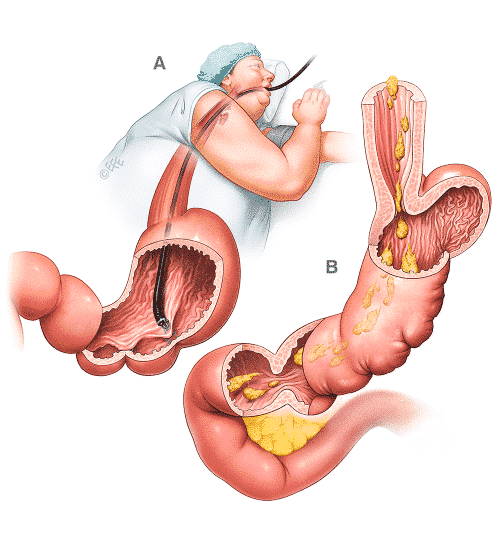
Endoscopic sleeve gastroplasty is done in the endoscopy unit as an outpatient procedure. General anesthesia is used for the procedure, so you’ll be unconscious.
The procedure is done using an endoscope, a flexible tube with a camera and an endoscopic suturing device attached. The endoscope is inserted down your throat into the stomach. The tiny camera allows the doctor operating the endoscope (endoscopist) to see and operate inside your stomach without making incisions in your abdomen.
Using the endoscope, the doctor places approximately 12 sutures in the stomach. The sutures change the structure of your stomach, leaving it shaped like a tube. This restricts the amount of calories your body absorbs.
The procedure takes about 90 minutes. After the endoscopic sleeve gastroplasty, you’ll awaken in a recovery room, where medical staff monitors you for any complications.
The majority of people leave go home the same day after recovering from sedation. Some people might require a short admission to the hospital for one day or less for observation after the procedure.
After Apollo endoscopic sleeve gastroplasty
After the procedure, you generally won’t be allowed to eat for about eight hours. Then, you’ll be allowed to start a liquid diet, which you need to continue for at least two weeks. Over four weeks, you’ll move on to semi-solid foods, and then to a regular healthy diet.
You’ll also have medical checkups and meet with a nutritionist and psychologist frequently after your procedure.
Results
Endoscopic sleeve gastroplasty can lead to significant weight loss. The amount of weight you lose also depends on how much you can change your lifestyle habits.
But studies have shown promising results. A recent study of people with an average BMI around 38 found that endoscopic sleeve gastroplasty led to an average weight loss of 39 pounds (17.8 kilograms) after 6 months. After 12 months, weight loss was 42 pounds (19 kilograms).
In a study of people with an average BMI of about 45, the procedure resulted in an average weight loss of about 73 pounds (33 kilograms) during the first six months.
As with other procedures and surgeries that lead to significant weight loss, endoscopic sleeve gastroplasty may improve conditions often related to being overweight, including:
- Gastroesophageal reflux disease
- Heart disease or stroke
- High blood pressure
- Severe sleep apnea
- Type 2 diabetes
The evidence we have suggests people can expect to lose about 15-18% of their starting weight (generally half of their excess weight) over a 12-18 month period*. At this stage, because this is still a new procedure, longer term weight loss results are not available.
The weight loss results in the chart below are the published results from a study of 248 ESG patients. They show average total body weight loss (TBWL) as a percentage of the starting weight. Also, we’ve shown how much weight this equates to assuming different starting weights.
In summary, based on the published data you can expect to lose just over half of your excess weight after 24 months. This is similar to the weight loss with a gastric band but as we said above, the latest results with the new technique are comparable to surgical sleeve and bypass.
| Weight loss | |||
| % of starting weight | Start weight 16st | Start weight 20st | |
| At 6 months | 15.2%* | 34lbs | 43lbs |
| At 18 months | 18.6%* | 42lbs | 52lbs |
Based on a group of 248 patients with a mean starting BMI of 37.8
Here is a summary of published weight loss data:
| Participants | Avg weight loss at 2 years | |
| Alqahtani et al | 1600 | 15-20% |
| Lopez-Nava et al | 248 | 18.6% |
| Sharaiha et al | 91 | 20.9% |
In the Lopez Nava study we saw that nearly all of the weight loss was achieved in the first 6 months
In February 2019 Apollo Endosurgery, Inc., a global leader in less invasive medical devices for bariatric and gastrointestinal procedures, announced the publication of Outcomes of Endoscopic Gastroplasty (“ESG”) in 1,000 Consecutive Patients from a single center – King Saud University, Riyadh, Saudi Arabia featured in Gastrointestinal Endoscopy (GIE) – https://doi.org/10.1016/j.gie.2018.12.012.
According to this publication, in these first 1,000 consecutive patients that treated with Endoscopic Sleeve Gastroplasty, patients experienced a 100% remission for hypertension related comorbidities, a 70% remission rate for type 2 diabetes with the remaining 30% showing significant improvement. Study confirmed that ESG is a safe, well-tolerated, and effective procedure. In addition, patients also achieved 64.7% excess weight loss at 18 months follow-up, which is comparable to results achieved with other surgical bariatric interventions.
When weight-loss surgery doesn’t work
It’s possible to not lose enough weight or to regain weight after any type of weight-loss procedure, even if the procedure itself works correctly. This weight gain can happen if you don’t follow the recommended lifestyle changes. To help avoid regaining weight, you must make permanent healthy changes in your diet and get regular physical activity and exercise.
Apollo Endoscopic Sleeve Gastroplasty
VISUAL SUMMARY
References:
1-Diet, nutrition and the prevention of chronic diseases. World Health Organ Tech Rep Ser 2003;916:i-viii,1-149.
2-Hiatt WR, Thomas A, Goldfine AB. What cost weight loss? Circulation 2012;125:1171-7. DOI: 10.1161/CIRCULATIONAHA.111.023499
3-Middleton KM, Patidar SM, Perri MG. The impact of extended care on the long-term maintenance of weight loss: A systematic review and meta-analysis. Obes Rev 2012;13:509-17. DOI: 10.1111/j.1467 789X.2011.00972.x
4-Chang SH, Stoll CR, Song J, et al. The effectiveness and risks of bariatric surgery: An updated systematic review and meta-analysis, 2003-2012. JAMA Surg 2014;149:275-87. DOI: 10.1001/jamasurg.2013.3654
5-ASGE/ASMBS Task Force on Endoscopic Bariatric Therapy, Ginsberg GG, Chand B, et al. A pathway to endoscopic bariatric therapies. Gastrointest Endosc 2011;74:943-53. DOI: 10.1016/j.gie.2011.08.053
6-Espinet-Coll E, Nebreda-Durán J, Gómez-Valero JA, et al. Current endoscopic techniques in the treatment of obesity. Rev Esp Enferm Dig 2012;104:72-87. DOI: 10.4321/S1130-01082012000200006
7-ASGE Bariatric Endoscopy Task Force; ASGE Technology Committee. Abu Dayyeh BK, Edmundowicz SA, Jonnalagadda S, et al. Endoscopic bariatric therapies. Gastrointest Endosc 2015;81:1073-86. DOI: 10.1016/j.gie.2015.02.023
8-Abu Dayyeh BK, Rajan E, Gostout CJ. Endoscopic sleeve gastroplasty: A potential endoscopic alternative to surgical sleeve gastrectomy for treatment of obesity. Gastrointest Endosc 2013;78:530-5. DOI: 10.1016/j.gie.2013.04.197
9-López-Nava G, Bautista-Castaño I, Jiménez A, et al. Endoscopic sleeve gastroplasty: How I do it. Obes Surg 2015;25:1534-8. DOI: 10.1007/ s11695-015-1714-7
López-Nava G, Galvão MP, Bautista-Castaño I, et al. Endoscopic sleeve gastroplasty for the treatment of obesity. Endoscopy 2015;47:449-52.
10-Sharaiha RZ, Kedia P, Kumta N, et al. Initial experience with endoscopic sleeve gastroplasty: Technical success and reproducibility in the bariatric population. Endoscopy 2015;47:164-6.
11-Gaur S, Levy S, Mathus-Vliegen L, et al. Balancing risk and reward: A critical review of the intragastric balloon for weight loss. Gastrointest Endosc 2015;81:1330-6. DOI: 10.1016/j.gie.2015.01.054
12-Dumonceau JM. Evidence-based review of the Bioenterics intragastric balloon for weight loss. Obes Surg 2008;18:1611-7. DOI: 10.1007/ s11695-008-9593-9
13-López-Nava G, Rubio MA, Prados S, et al. BioEnterics® intragastric balloon (BIB®). Single ambulatory center Spanish experience with 714 consecutive patients treated with one or two consecutive balloons. Obes Surg 2011;21:5-9. DOI: 10.1007/s11695-010-0093-3
14-López-Nava G, Bautista-Castaño I, Jiménez-Baños A, et al. Dual intragastric balloon: Single ambulatory center Spanish experience with 60 patients in endoscopic weight loss management. Obes Surg 2015;25:2263-7. DOI: 10.1007/s11695-015-1715-6
15-Angrisani L, Lorenzo M, Borrelli V, et al. Is bariatric surgery necessary after intragastric balloon treatment? Obes Surg 2006;16:1135-7. DOI: 10.1381/096089206778392365
16-Abu Dayyeh BK, Kumar N, Edmundowicz SA, et al.; ASGE Bariatric Endoscopy Task Force; ASGE Technology Committee. ASGE Bariatric Endoscopy Task Force systematic review and meta-analysis assessing the ASGE PIVI thresholds for adopting endoscopic bariatric therapies. Gastrointest Endosc 2015;82:425-38.e5. DOI: 10.1016/j.gie.2015.03.1964
17-ASGE Bariatric Endoscopy Task Force, Sullivan S, Kumar N, et al. ASGE position statement on endoscopic bariatric therapies in clinical practice. Gastrointest Endosc 2015;82:767-72. DOI: 10.1016/j. gie.2015.06.038
18-Espinós JC, Turró R, Mata A, et al. Early experience with the Incisionless Operating Platform (IOP) for the treatment of obesity: The Primary Obesity Surgery Endolumenal (POSE) procedure. Obes Surg 2013;23:1375-83. DOI: 10.1007/s11695-013-0937-8
19-López-Nava Brevière G, Bautista-Castaño I, Jiménez A, et al. The Primary Obesity Surgery Endolumenal (POSE) procedure: Oneyear patient weight loss and safety outcomes. Surg Obes Relat Dis
2015;11:861-5. DOI: 10.1016/j.soard.2014.09.026
20-Ministerio de Sanidad, Servicios Sociales e Igualdad: Estrategia para el Abordaje de la Cronicidad en el Sistema Nacional de Salud. Ed. Ministerio de Sanidad, Servicios Sociales e Igualdad. Madrid; 2012. Disponible en:http://www.observatorio.naos.aesan.msssi.gob.es/docs/docs/documentos/estrategia_pa_el_abordaje_de_la_cornicidad_en_el_ sistema_nacional_de_salud_2012.pdf (acceso 12-3-2015).
Ministerio de Sanidad, Política Social e Igualdad: Plan de Calidad para el Sistema Nacional de Salud 2010. Disponible en: http://www.msssi. gob.es/organizacion/sns/planCalidadSNS/pdf/pncalidad/PlanCalida 2010.pdf (acceso 12-3-2015).




